To the Editor:
Lung injury associated with vaping — the use of electronic nicotine delivery systems (ENDS) — has been recognized in the medical literature,1,2 and a case series of such injuries is now published in the Journal.3 If vaping is the proximal cause of lung injury, the mechanism leading to such injury is not certain. Unlike traditional cigarettes, ENDS use solvents to heat and aerosolize the flavorants (known as “juices”),4 which consist of various aldehydes and alcohols, and complications can arise as the mixing and aerosolization of these components create new compounds. Moreover, ENDS are increasingly used to deliver cannabis oils and concentrates.
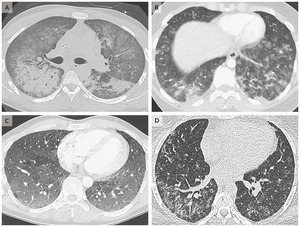
An image obtained from a 20-year-old man with diffuse alveolar damage (Panel A) shows dependent consolidation and diffuse ground-glass opacity, with some areas of bronchial dilatation typical of diffuse alveolar damage. The patient underwent intubation on hospital day 2 but eventually recovered after receiving glucocorticoid therapy. An image obtained from a 19-year-old woman with acute eosinophilic pneumonia (Panel B) shows diffuse nodular areas of consolidation and ground-glass opacity, with mild septal thickening and a small right pleural effusion. The findings cleared within days after the administration of glucocorticoids. An image obtained from a 35-year-old man with a pattern of hypersensitivity pneumonitis (Panel C) shows extensive centrilobular ground-glass attenuation nodules, especially in the anterior region, and more confluent ground-glass opacity in the dependent lungs, with lobules of mosaic attenuation. The patient’s symptoms improved after cessation of vaping. An image obtained from a 49-year-old woman with giant-cell interstitial pneumonia (Panel D), which was diagnosed on the basis of findings on surgical biopsy of the lung and was attributed to cobalt in her vape pen, shows fibrosis characterized by peripheral reticulation, ground-glass opacity, and mild traction bronchiectasis. The patient’s symptoms improved after cessation of vaping.
We have collectively seen 19 cases and reviewed the literature regarding another 15 cases. All met the case definition of vaping-associated lung injury, which includes “abnormalities on chest imaging.” We identified four imaging patterns that correlated with pathological findings attributable to vaping, including acute eosinophilic pneumonia, diffuse alveolar damage, organizing pneumonia, and lipoid pneumonia. In addition, some cases were associated with variegated imaging patterns. Through clinical and pathological investigations, patterns of giant-cell interstitial pneumonia, hypersensitivity pneumonitis, and diffuse alveolar hemorrhage were identified (Figure 1; and see the Supplementary Appendix, available with the full text of this letter at NEJM.org).
Although the variety of imaging patterns suggests different mechanisms of injury, and more patterns will probably be reported, most of the patterns have basilar-predominant consolidation and ground-glass opacity, often with areas of lobular or subpleural sparing. Rapidly developing acute lung injuries (e.g., acute eosinophilic pneumonia and diffuse alveolar damage) are associated with inhalational injuries and have overlapping pathological and imaging findings,5 and they have been reported to occur with vaping.1 Hypersensitivity pneumonitis is an immune response to an environmental antigen, but the antigens related to vaping are unknown. Lipoid pneumonia is an inflammatory response to the presence of lipids within the alveolar space and typically results from aspiration of hydrocarbons or oil-based products, but it has now been seen with vaping. We have not observed the computed tomographic finding of fat attenuation in the lung, which is a hallmark of lipoid pneumonia, in these cases of vaping-associated lung injury. Not all cases are acute; organizing pneumonia often develops subacutely, over a period of days to weeks, and the one case of giant-cell interstitial pneumonia (a rare fibrosing interstitial lung disease) that was correlated with hard metals in ENDS developed over a period of 6 months.
Travis S. Henry, M.D.
University of California, San Francisco, San Francisco, CA
Jeffrey P. Kanne, M.D.
University of Wisconsin School of Medicine and Public Health, Madison, WI
Seth J. Kligerman, M.D.
University of California, San Diego, San Diego, CA
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
This letter was published on September 6, 2019, at NEJM.org.
1. Arter ZL, Wiggins A, Hudspath C, Kisling A, Hostler DC, Hostler JM. Acute eosinophilic pneumonia following electronic cigarette use. Respir Med Case Rep 2019;27:100825–100825.
2. Viswam D, Trotter S, Burge PS, Walters GI. Respiratory failure caused by lipoid pneumonia from vaping e-cigarettes. BMJ Case Rep 2018;2018:224350–224350.
3. Layden JE, Ghinai I, Pray I, et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin — preliminary report. N Engl J Med. DOI: 10.1056/NEJMoa1911614
4. Jensen RP, Strongin RM, Peyton DH. Solvent chemistry in the electronic cigarette reaction vessel. Sci Rep 2017;7:42549–42549.
5. Kligerman SJ, Franks TJ, Galvin JR. From the radiologic pathology archives: organization and fibrosis as a response to lung injury in diffuse alveolar damage, organizing pneumonia, and acute fibrinous and organizing pneumonia. Radiographics 2013;33:1951–1975.
This content was originally published here.
EL 2 DE JUNIO DEL 2024 VOTA PARA MANTENER
TU LIBERTAD, LA DEMOCRACIA Y EL RESPETO A LA CONSTITUCIÓN.
VOTA POR XÓCHITL